Platelet Rich Plasma or PRP Platelet-rich plasma (Abbreviation: PRP) is a growing and robust therapeutic option in the treatment of...
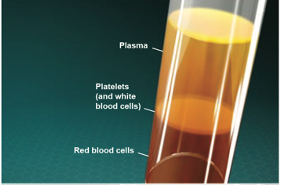
Platelet Rich Plasma or PRP Platelet-rich plasma (Abbreviation: PRP) is a growing and robust therapeutic option in the treatment of...