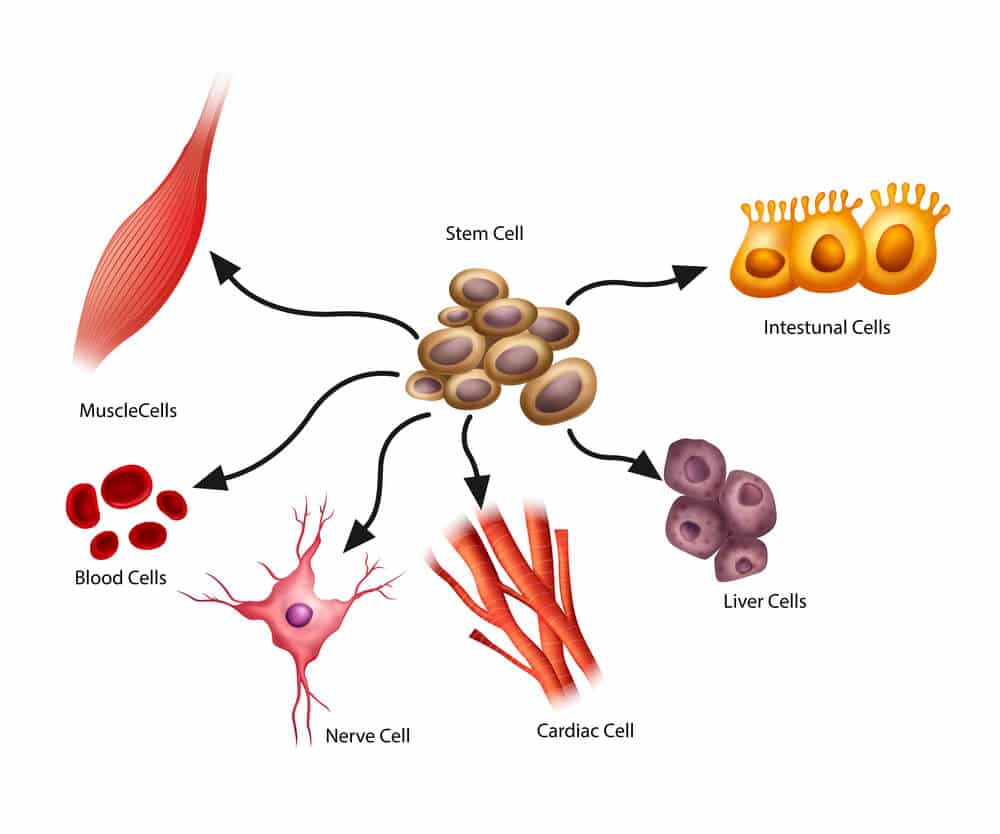
Stem cells are just one of the 210 cell types that make up the human body. We learned in Stem Cell Therapy Clinical Applications that stem cells possess two unique features that distinguish them from all other cells in the body. Stem cells can divide and continually renew themselves for a long period of time (stem cells theoretically are immortal, but not so in reality). Secondly, stem cells have the capability to give rise to the 209 more specialized cells types (differentiation).
You probably have seen more articles on stem cells as of late. Why the interest? Stem cells are used to repair and regenerate the body. If we did not have stem cells it is estimated that we would one live one or two days. Our longevity is largely determined by the quality and quantity of our stem cells. We can now use our own stem cells to treat disease and improve our health.
Discussions on stem cells can be confusing and it helps to use clear defined terms and part of that is understanding how stem cells are classified. There are three main stem cell classification systems.
Stem Cell Classification
Stem cells can be classified based on their origin, potency, and source.
Origin has to do with stage of human development from which stem cells are being harvested. Potency has to do with the ability of a stem to differentiate into the other 209 cell types. And, source has to do with whether the stem cells are coming from one’s self, another individual, or possibly even a different species.
Here is how these stem cell classification system works in reality. Adult stem cells are multipotent and can be used for autologous transplants (one’s own stem cells) or used in allogeneic transplantations (transplanted into another person). Embryonic stem cells are pluripotent and are used in allogeneic transplants (they cannot be used for autologous stem cell transplantation since the embryo is no longer alive). While this may seem confusing, it should become more clear by the end of this article.
Let’s go through each classification system first before providing more detail.
Origin
- Embryonic
- Fetal
- Adult
- IPS (induced pluripotent stem cells)
Potency
- Totipotent
- Pluripotent
- Multipotent
- Oligopotent
- Unipotent
Source
- Autologous
- Allogeneic
- Xenogeneic
Development of Human Embryo
After fertilization of a human egg with a sperm the resulting zygote begins to divide first into two cells then into four cells then into eight cells (all these cells are alike). That takes about three days. Then around day four those eight cells divide into 16 cells called a morula – a solid ball of cells contained within the zona pellucida. Up to that point each of those cells is totipotent having the capability of producing a fetus. Identical twins are an example where early on two fetuses develop from a single egg and sperm.
On day five the morula gives rise to a blastocyst and the cells are no longer clumped together like grapes (morula). Instead the cells begin to organize while a cavity develops in the zona pellucida. At this point the cells are no longer totipotent and are now pluripotent with the potential to differentiate into almost any of the other 209 cell types forming the human body, but no longer can give rise to complete fetus or organism. It is at this stage that human embryo stem cells are derived or harvested.
Legality of Embryonic Stem Cells
Here’s a brief history on the legality and funding of embryonic research as there is some confusion on this within the general public. Research on embryonic stem cells was never banned or illegal. The question and debate have been about the federal funding of research on embryonic stem cells.
Embryonic stem cells are derived from unwanted embryos from in-vitro fertilization clinics. President George W. Bush on August 9, 2001 allowed for federal funds for research only on the 21 existing human embryonic stem cell lines in existence prior to August 9, 2001. But, federal funds could not be used to create new embryonic stem cells line after that date. Since embryonic stem cells can divide continuously in laboratory environment, one embryonic stem cell line should sufficient enough to conduct research. At least, that was part of the thinking in not needing additional embryonic stem cell lines.
Prior to President Bush’s decision no federal funding was allowed on embryonic stem cells. This is interesting as President Bush is often portrayed as hampering research on embryonic stem cells, when it fact, he opened the door for federal funding of it – just not new embryonic lines. Even though he allowed for some federal funding his decision did not go as far as many researchers were hoping. Prior to President Bush’s decision, President Clinton allowed for federal funding for research on aborted fetal stem cells but not embryonic stem cells. President Obama subsequently allowed for federal funding for broader research on embryonic stem cells loosening some of the restrictions imposed by President Bush.
Some of these issues regarding federal funding of stem cell research are less relevant in reality as embryonic stems cells have little clinical application advantage (perhaps that will change in the future) in treating adult disorders over adult stem cells, though embryonic stem cells do hold vast research interest.
 Stem Cell Classification: Origin
Stem Cell Classification: Origin
Now we will review stem cell classification from an origin perspective while adding discussions on potency and source classifications as we go along.
Embryonic
We discussed the highlights of embryonic stem cells in the above sections. Embryonic stems cells are pluripotent (which is not as desirable as it may seem on the surface). Again, this means embryonic stem cells can differentiate into the other 209 more specialized cells. They are relatively easy and inexpensive to obtain compared to harvesting adult stem cells.
But, their use comes with some risk. These include the risk that the recipient of embryonic stem cells could inherit a genetically based disease that the embryo carries. Another challenge is getting embryonic stem cells to actually differentiate into the cells/tissue desirable. There is also the risk of uncontrolled growth of embryonic stem cells in the host or recipient leading to cancers. Embryonic stem cells carry the risk of immune rejection as seen in transplanted organs (kidney and hearts) as well.
And, of course there are the obvious ethical concerns in sacrificing a life to obtain stem cells.
None of those risks or concerns exist when adult stem cells are harvested and then reintroduce into the same individual (in other words – when a person receives his/her own stem cells).
Fetal
Fetal stem cells were used in humans as early as 1982 to treat Parkinson’s disease. This was before the potential of adult stem cells was realized. Fetal stem cells are harvested from aborted fetuses and share the same ethical concerns as embryonic stem cells. They are easy to obtain (harvest) like embryonic cells. They are multipotent unlike embryonic stems which are pluripotent. This means fetal stem cells self-renew but can only differentiate into a certain number of closely related tissues cells. Hematopoietic stem cells will differentiate into the various blood cells – red blood, white blood cells, and platelets but nothing else. And, mesenchymal stem cells will differentiate into muscle, bone, cartilage, and connective tissue, for instance.
Oligopotent stem cells differentiate into just a couple different cell types and unipotent stem cell only differentiate into a single cell type like muscle satellite stem cells.
Adult Stem Cells
We will be spending more time discussing adult stem cells in future articles and will just cover the basics here. Adult stem cells are multipotent. They are typically harvested from bone marrow and adipose (fat) tissue. Compared to embryonic and fetal stem cells, adult stem cells are more difficult to obtain, though still relatively easy. They are found in fewer numbers, though, which may hamper their use the older we become. Much of the success in any stem cell transplantation is simply related to the number of stem cells transplanted. The more stem cells that have been transplanted and stimulated to differentiate the better the success. In that regard, embryonic and fetal stem cells have a numbers advantage over adult stem cells, but in most cases enough adult stem cells can be harvested to treat adult conditions adequately.
In treating adult conditions it is actually more desirable to use multipoint stem cells than pluripotent stem cells. This may seem opposite of what one might think. The reason for that is you want to use stem cells that are already predetermined to repair the type of tissue in need of repair. You want to use cells that are already a closely related to the cell or tissue desired, so to speak. That’s one reason why the pluripotent embryonic stem cells have little clinical advantage over adult stem cells.
Individuals can donate their stem cells for their own use (present use, or future use through stem cell banking). Autologous stem cell transplants occur when stem cells are harvested and then given back to the same person. Or, stem cells can be harvested, donated, and used to treat another human being. This is often the case in bone marrow transplants used to treat leukemias. This is called allogeneic stem cell transplantation.
Xenogeneic transplantation occurs when tissue from an animal is transplanted into another type of animal or even a human. Transplantation of a pig or cow heart valve into a human is an example of xenogeneic transplantation. Bone cellular products used to treat fractures that failed to heal come from animals in some cases.
Induced Pluripotent Stem Cells
Induced pluripotent stem cells may be the most fascinating of stem cells. They are of much research interest. Induced potent stem cells are regular cells (usually fibroblasts) that have been reprogrammed back to becoming pluripotent stem cells. In theory any of the other 209 types of cells can be reprogrammed into induced pluripotent stem cells. They are of research interest because if they can successfully be used in humans that would minimize the “need” and ethical concerns related embryonic stem cells which are also pluripotent.
The problem with induced pluripotent stem cells is it is unclear whether such cells retain some “memory” of what they used to be. For instance, would a fibroblast that was induced to become a neural stem cell revert back to a fibroblast at some later date? Also, the factors and techniques that are used to reprogram cells involve the use of oncogenes (cancer genes) and viruses both of which would be transmitted to the host.
Fairly recently though, mice and rat fibroblasts were reprogrammed to become Leydig cells (testosterone producing cells) and were used to treat rodents with low testosterone. See Stem Cell Treatment for Low Testosterone – Can it be Done?
Through stem cells the body repairs itself. Everyday the body experiences microtrauma, oxidation, degeneration, and physical insults to its various tissues. Hopefully, your understanding of stem classification is more clear than it was at the beginning of this article. Knowing these stem cell classification terms will be helpful as we go into depth about stem cell therapy and its potential in treating a variety of human conditions that we will discuss in future articles.
